Navigating Consumer Expectations in Healthcare: Insights from the 2024 Healthcare Consumer Survey
Transformation throughout the healthcare industry is reshaping the relationship between consumers and their health plans. Consumers are demanding more personalized and dynamic experiences, making it crucial for health plans to adapt and respond effectively.
The 2024 HealthEdge® Consumer Survey provides valuable insights into these shifting dynamics in health. With over 3,500 healthcare members participating, the consumer survey sheds light on the member expectations and satisfaction levels. This comprehensive analysis not only underscores opportunities in a changing landscape but also highlights how HealthEdge solutions can empower health plans to address these changes and ultimately enhance member satisfaction.
Member Voices: Health Plans Get High Marks with Room for Growth
The consumer survey revealed some interesting findings regarding member satisfaction and expectations:
- High Satisfaction Rates: A significant 69% to 86% of members reported being “very satisfied” or “satisfied” with their health plans, particularly those in Dual-eligible and Medicare Advantage programs.
- Early Intervention: Members want a more proactive and preventative approach from their health plans. This includes a focus on preventative care, cost transparency, and improved care coordination.
- Digital Tool Adoption: A substantial 65% of members are comfortable using digital tools such as mobile apps and AI-powered solutions to interact with their health plans.
- Potential for Churn: About one-third of the surveyed members indicated a likelihood of switching their health plans within the next year, especially those with individual or employer-sponsored coverage.
These findings show a clear trend: consumers are actively seeking more engaged, transparent, and personalized healthcare experiences. Health plans that prioritize these areas will be well-positioned to not only maintain satisfaction but also build stronger member relationships.
A Demand for More Personalized and Proactive Healthcare
Today’s healthcare consumers are no longer passive recipients of medical coverage. They demand a service that is personalized, proactive, transparent, and convenient. The main factors driving these expectations include:
- Expanded Selection: The expansion of options through the ACA Marketplace and Medicare Advantage empowers consumers to shop around for plans that best meet their needs.
- Digital Fluency: As everyday activities shift online, consumers expect their health plans to offer similar digital conveniences.
- Cost Awareness: With rising healthcare costs, consumers emphasize the importance of financial transparency and affordability in their health plans.
- Regulatory Shifts: Recent regulations have enhanced patients’ access to their medical records, encouraging deeper engagement in their health decisions.
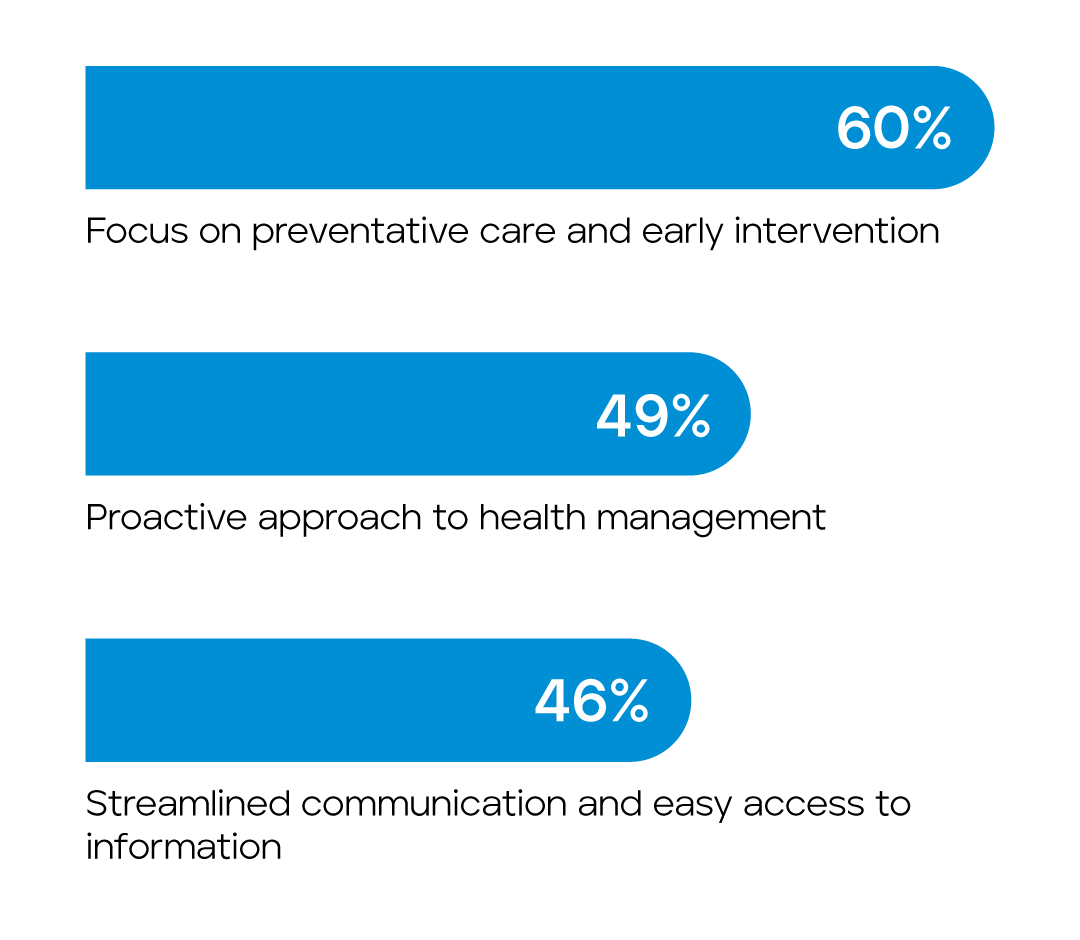
The full research report dives deeper into the satisfaction levels of different member populations, the likelihood of members switching health insurance plans in the coming year, and the expectations that consumers have for their health plans. It also describes what “personalized healthcare experience” means to most consumers, which includes:
- 60% – Focus on preventative care and early intervention
- 49% – Proactive approach to health management
- 46% – Streamlined communication and easy access to information
A dedicated section of the report examines how care management teams can enhance member satisfaction, noting that only 36% of those assigned a care manager were fully satisfied with their care management. Despite care managers’ extensive responsibilities, which include care coordination, medication management, and care plan development, members want more individualized care that meets their unique needs.
Modern solutions, like those offered by HealthEdge®, are essential in meeting the rising demand for more personalized experiences and engagement between members and their health plans.
How HealthEdge® Supports Payers in Elevating Member Experience
At HealthEdge, our mission is to innovate a world where healthcare can focus on people. That’s why we offer integrated software solutions designed specifically for modern healthcare consumers. These solutions enable us to work together with members and care managers to create personalized care plans, ultimately fostering a more people-centric healthcare experience.
- Empowering with Technology: HealthEdge’s platforms, such as the GuidingCare® care management suite and the Wellframe
 digital engagement platform, integrate seamlessly to empower members, care managers, and payers with more personalized care. Features like one-click referrals, real-time data access, and personalized content delivery significantly enhance the member experience while reducing the administrative burdens on care managers.
digital engagement platform, integrate seamlessly to empower members, care managers, and payers with more personalized care. Features like one-click referrals, real-time data access, and personalized content delivery significantly enhance the member experience while reducing the administrative burdens on care managers. - Improving Transparency and Convenience: HealthEdge solutions support the Transparency in Coverage Act requirements, providing members with real-time cost-sharing estimates and comprehensive access to their health plan information through user-friendly portals and mobile applications.
- Supporting Personalized Care: The solutions support personalized care management, enabling health plans to effectively and proactively address and fulfill individual member needs. This tailored approach is crucial for boosting member satisfaction and fostering loyalty.
Moving Forward: Health Plans as Partners in Care
The survey’s insights reveal a crucial shift in the healthcare sector: members no longer see health plans merely as payers but as partners in their health journey. They expect proactive guidance and personalized support from their health plans.
To stay relevant and competitive, health plans must adopt advanced solutions like those offered by HealthEdge to meet these expectations. These modern solutions facilitate proactive, personalized engagement, allowing plans to offer the kind of service that consumers now demand. Furthermore, the integration of care management and member engagement solutions optimizes operational processes and enhances member satisfaction through improved services. This translates to a win-win for both health plans and members.
As the healthcare landscape continues to evolve, so do consumer expectations. The 2024 HealthEdge® Consumer Survey highlights a critical trend in healthcare: the need for health plans to adopt a more personalized, informed, and technology-driven approach to member engagement and satisfaction.
Don’t let your health plan get left behind! HealthEdge is at the forefront of this transformation. We offer the modern solutions you need to meet and exceed these evolving demands. Uncover the data behind the member voices. Download the full 2024 Consumer Survey report today.

