Regulatory Highlights that Health Plans Should Know
The Patient Access API and the Provider Directory API will be enforceable on July 1, 2021. HealthEdge is confident that we will have our standardized data requirements to enable the plans to have full compliance.
Currently, plans are likely focused on the member portal technology, authentication, and authorization management. We have ensured that the data that we routinely move provides them everything they need for the FHIR-enabled data store.
The Payer-to-Payer Data Exchange is the heavier lift. While our current APIs will handle the data extraction, there is also an ingestion aspect of the data exchange. On January 1, 2022, health plans will likely just hold the data in a data warehouse. Beyond accepting an electronic file for a new member, the Rule does not yet outline how to ingest and use the information. There will be a translation process, but by building upon the x12 inbound transaction processing the path is already paved.
We expect to see some business cases for the use of historical data in 2021. HealthEdge is prepared to dig into those business cases as they develop looking for some synergy between what we do and what plans need.
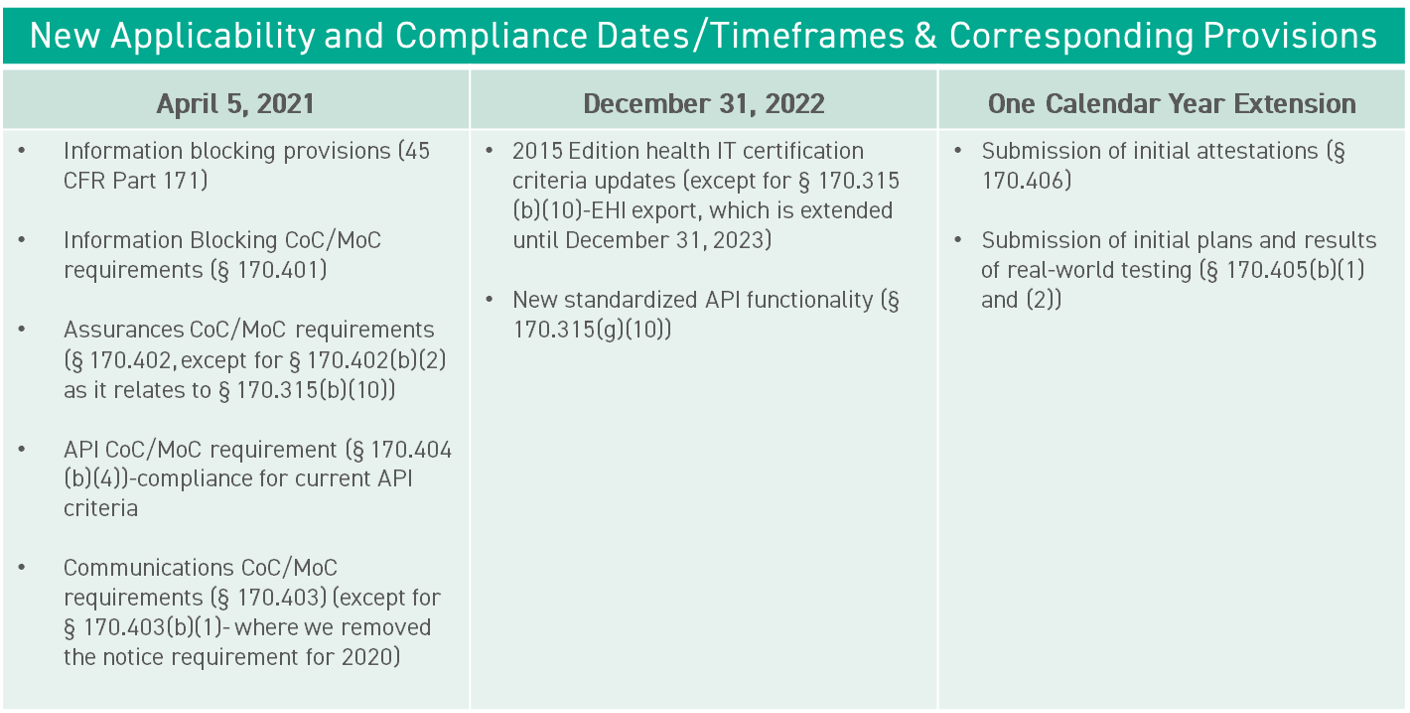
ONC Final Rules on Information Blocking & HIT Certification
The ONC Information Blocking Final Rule was to become enforceable on November 2, 2020. However, due to COVID-19 and other current initiatives, ONC did not believe it was feasible to enforce the Rule and announced in late October that it would delay implementation.
ONC has released new dates and timeframes beginning on April 5, 2021.
Transparency in Coverage – Final Rule
The Transparency in Coverage Final Rule has been published and becomes effective on January 11, 2021.
On January 1, 2022, health plans must post and regularly update machine-readable files, to the plan’s public website, of in-network negotiated provider rates, in-network drug pricing, and out-of-network coverage rates.
On January 1, 2023, health insurance providers must offer an online shopping tool or similar platform that includes out-of-pocket cost estimates and negotiated prices for 500 of the “most shoppable” services (which are yet to be defined). We think there is potential to use trial claim functionality in HealthRules® Payor for this type of shopping tool. On January 1, 2024, the 500 cap is removed and online shopping must expand to all services.
In the tool, a user would log in to see their estimated cost-sharing, including what provider they want to go to, what service they need, and where that procedure might happen. There are still a lot of questions around this. At this point, the identification of the risk factors is up for debate. Most users will not have the CPT billing code or NDC – National Drug Code . They will not know whether there’s bundled services or not. There needs to be logic that explains how to display cost estimates for desired services.
Additionally, as health plans calculate their 2020 Medical Loss Ratio (MLR) reporting year, they can include any shared savings payment that the issuer has made to an enrollee due to the member choosing to obtain health care from a lower cost, higher value provider.
HIPAA Transactions and Code Sets (EDI)
The current version (5010) of the X12 HIPAA Transaction has been in use for about 10 years. Looking back over the timeline of HIPAA EDI, spanning the past 17 years, we implemented the Rule using V4010 and upgrade it to V5010 to support ICD-10. The functionality of newer versions is needed and the National Committee on Vital and Health Statistics’ (NCVHS) and the Department of Health and Human Services have been in discussions for some time about adopting a newer version of the X12N HIPAA EDI Transactions.
X12 has been working on Version 7030 for several years as the next version to be adopted under HIPAA.
X12 works with the industry subject matter experts to develop implementation guides that meet the needs of the industry within the guidelines of HIPAA.
Recently, X12 announced that the completed V7030 implementation guides would form the basis of Version 8010, meaning we are a long way towards a completed Version 8010. It is expected that X12 will recommend to NCVHS that we skip 7030 and go directly to version 8010 as the next HIPAA transaction standard.
HealthEdge will continue monitoring this to determine the version and timeline for implementation.
Additional Policy and Regulatory Revisions in Response to the COVID– 19 Public Health Emergency
On November 6, 2020, the Tri-Agencies published an interim final rule (IFR) with request for comments about COVID-19 and the response. The effective date is January 1, 2021. HealthEdge has analyzed the IFR, and it does not appear that any significant details have changed regarding zero cost-sharing for testing and treatment, etc.
We are getting close to a COVID-19 vaccine, and CMS has provided guidelines about how to handle claims for the vaccine, minimizing delays that sometimes happen with the issues around release of new vaccines.
The American Medical Association (AMA) who is responsible for CPT-4 codes, issued the new vaccines specific codes to report the immunization for COVID-19. There are codes for the vaccine products as well as vaccine administration.
AMA worked very closely with CMS to create these new vaccine administration codes so that they are distinct to each vaccine and the specific dose. This specificity will allow them to track each vaccine dose, even if the vaccine product is not reported through a claim (i.e., if the vaccine was given to the patient for free.)
CY2022 – Advance Notices
We received advanced notices for the calendar year 2022 for your Medicare Advantage (MA) and prescription drug information Part C and Part D Payment Policies.
On September 14, 2020, we received part one. CMS is proposing to fully transition to the risk adjustment model adopted in the 2020 rate announcement. CMS will announce the MA capitation rates and final payment policies no later than Monday, April 5, 2021.
On October 30, 2020, we received Part Two, which includes preliminary estimates for the national per capita MA growth percentages and national Medicare fee-for-services growth percentages, which are key factors in determining the MA capitation rates. CMS also announced some changes in the Part C payment methodology, as well as annual adjustments to Part D prescription drug benefit parameters, Medicare Advantage PD star ratings, and economic information for the significant provisions.
Our team is drilling down on these notices and will provide more information on the calendar year 2022.
CMS – Annual Enrollment Period
The CMS Annual Enrollment period is happening right now and ends on December 7, 2020.
Next important deadline is coming up on December 4, 2020 MLR (Medical Loss Ratio) data for 2019 must be submitted to CMS via HPMS.
