Streamline Healthcare Contract Negotiations and Reviews with HealthEdge Source™ What-If Modeling
Health plans face a variety of challenges when it comes to contract modeling, negotiations, and reviews. A reliance on manual processes and disparate tools can make it difficult to accurately evaluate the financial impacts of new provider contracts.
In a recent webinar, healthcare industry experts shared their experiences working with health plans to improve accuracy and scalability in the contract review process. This blog highlights key insights from the virtual session that can help transform hypothetical conversations into actionable, data-driven negotiations.
5 Challenges Health Plans Face During Contract Negotiations
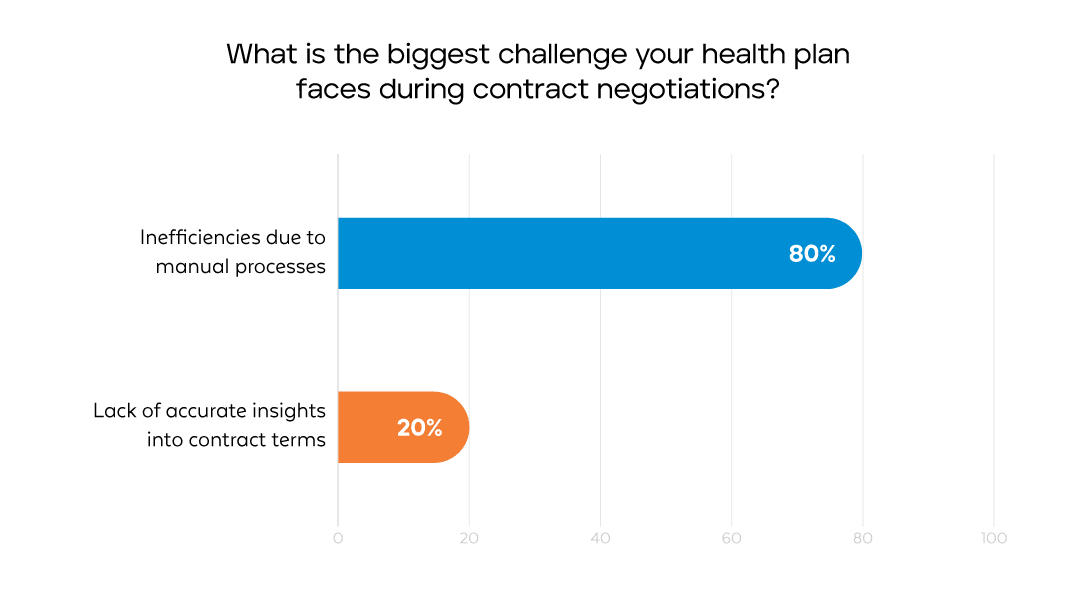
During the webinar, we polled the audience to better understand their major challenges. 80% of respondents said, “inefficiencies due to manual processes” were their primary concerns, followed by “lack of accurate insights into contract terms.”
What is the biggest challenge your health plan faces during contract negotiations?
1. Manual Processes: Many health plans still rely on outdated tools, such as spreadsheets and pivot tables, to model contract scenarios. These manual methods are error-prone, time-consuming, and inflexible, leading to delays in negotiations and decision-making.
2. Lack of Accurate Insights: Without timely and accurate information, health plans struggle to understand the financial implications of certain contract terms. This includes challenges in analyzing how payment term changes affect reimbursements or savings, hindering their ability to make informed decisions.
3. Disjointed Systems and Data Sources: The workflows for contract negotiations often involve disparate tools and systems. These siloed environments make it hard to analyze and reconcile data, leading to unnecessary complexity when assessing contractual impacts.
4. Configuration Challenges: After contracts are finalized, health plans sometimes discover that the terms cannot be efficiently configured into their existing claims processing systems, causing operational bottlenecks and delays in implementation.
5. Lag Time Between Contract Finalization and Execution: There is often a gap between signing a contract and getting it fully operational. This lag time can result in delays in reimbursement or improper payments, creating friction between stakeholders.
These challenges not only create inefficiencies that cost time and resources but also compromise the accuracy of contract modeling.
What-If Modeling: Our Vision for a Better Solution
At HealthEdge Source™, our team is developing a solution to eliminate these challenges by bringing advanced technology and seamless workflows into the contract negotiation process. The HealthEdge Source What-If Modeling tool will allow health plans to envision, evaluate, and execute contract scenarios with unprecedented precision.
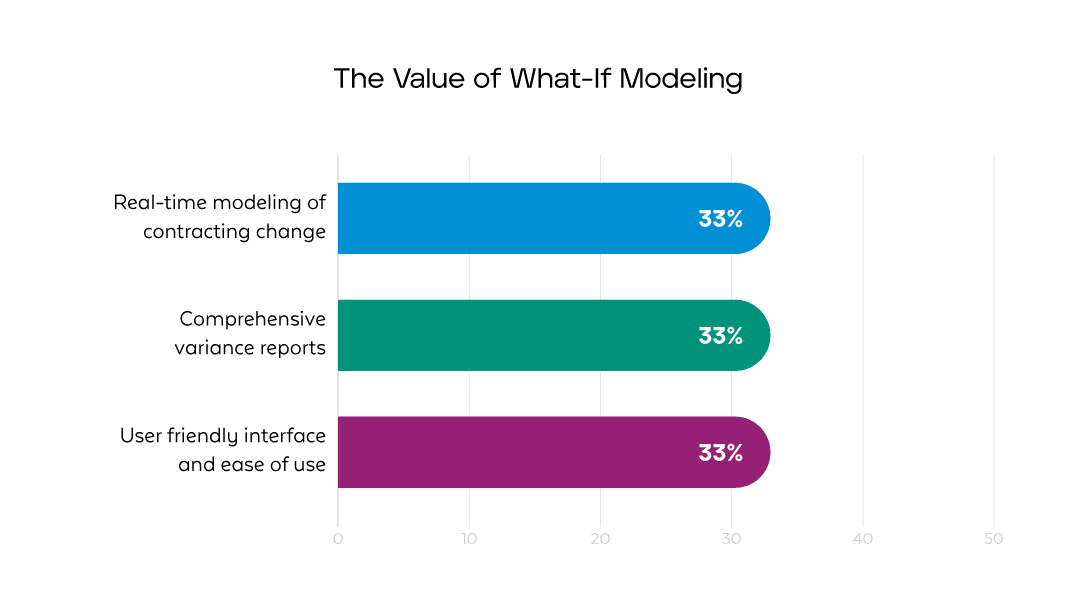
During the webinar, we demonstrated the solution and asked what participants found most valuable about the tool for their organizations. The top answers were:
Increasing Contract Value for Health Plans
- Automation and Real-Time Modeling: HealthEdge Source What-If Modeling is designed to replace manual processes with automated workflows, allowing health plans to build, test, and analyze contract configurations in minutes. Health plans will also be able to model complex scenarios in real time, significantly reducing the time and effort required to optimize contracts.
- Precision in Financial Insights: With penny-precise modeling for various reimbursement terms, health plans will be able to better anticipate the financial impacts of their contracts with greater accuracy, increasing confidence in projections and negotiations.
- Unified Platform for Disparate Processes: The new tool will bring together all critical functions—such as claims editing, pricing, and advanced analytics into a single platform. This will eliminate the need for multiple disparate systems and create a cohesive environment for assessing data and contracts.
- Self-Service Accessibility: With a user-friendly interface, the solution will empower contract negotiation teams to independently configure, compare, and adjust contract terms. Teams will be able to run “what-if” scenarios to evaluate potential impacts without relying on external support.
- Seamless Integration with Existing Systems: It will integrate smoothly as a modular component of HealthEdge Source. It can also function as a standalone system, allowing health plans to leverage the tool within their existing ecosystems.
- Reduced Lag Time: The tool will directly convert modeled contracts into production-ready configurations, significantly reducing the time needed to operationalize agreements. This will help ensure accurate reimbursements from the start, while preventing downstream inefficiencies and rework.
HealthEdge Source What-If Modeling will support various complex contract structures, including carve-outs for specific services (e.g., ER visits) or alternative payment models like capitation. These features were developed to make it easier for health plans to negotiate and model deals that align with their financial objectives and operational capacities.
Supporting a Collaborative Approach to Change
With the tool, health plans can bridge the gap between contracting and configuration teams, encouraging collaboration that helps determine whether contract terms are feasible. By identifying potential configuration issues during the modeling phase, health plans can minimize surprises and shorten implementation time. This approach can also help reduce provider abrasion and better inform contracting teams of the potential impact of custom configurations.
The Road Ahead for What-If Modeling
We invite you to watch the webinar recording to see a demo of the HealthEdge Source What-If Modeling tool in action and learn more about its functionalities. Discover how this innovative solution can transform your contract modeling process and deliver unparalleled precision and efficiency. Watch the webinar on-demand
Together, we can transform the way health plans approach contract modeling and create impactful results. If you’d like to contribute feedback or participate in our beta testing phase, we’d love to hear from you! Current customers can reach out to their Customer Success Managers for more information.