Take Control of Business Rules with Advanced Custom Edits
When it comes to claims processing, it’s easy to look at an error rate of 3-7% and be satisfied with your progress. But if you dig deeper, you may see a different, more concerning picture. Every year, health plans lose an estimated $86.49 billion dollars due to incorrect payments. Don’t get stuck spending valuable resources on just managing and reconciling data.
Ensuring payment integrity in healthcare is essential, but the process is full of hurdles and can be costly. You might find your health plan fighting against outdated or inaccurate edits, depending too heavily on external vendors, held back by a lack of customization and flexibility in your payment processes, and stuck in slow development cycles. These issues aren’t just annoying—they can lead to mistakes, inefficiencies, compliance risks, and a lot of frustration for both your members and providers.
Common Claims Editing Challenges for Health Plans
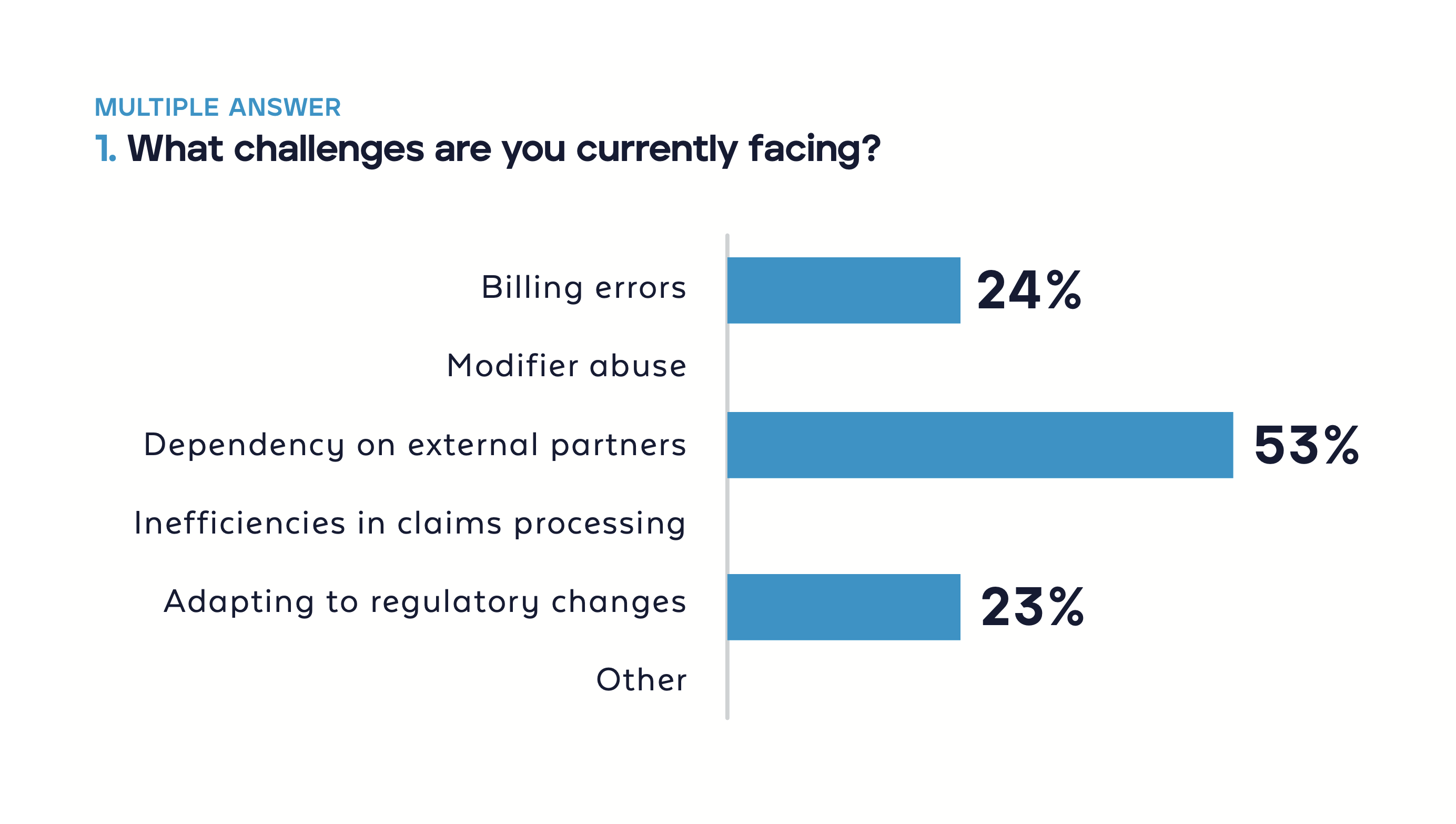
In a recent webinar, a HealthEdge® expert discussed how health plans can take control of business rules and create their own edits to improve claims processing. During the webinar, our audience reported that some of their biggest challenges include: relying on external partners, billing errors, and keeping up with regulatory changes.
These responses demonstrate health plan needs for more adaptable solutions, less reliance on third-party vendors, and staying up-to-date with regulatory changes.
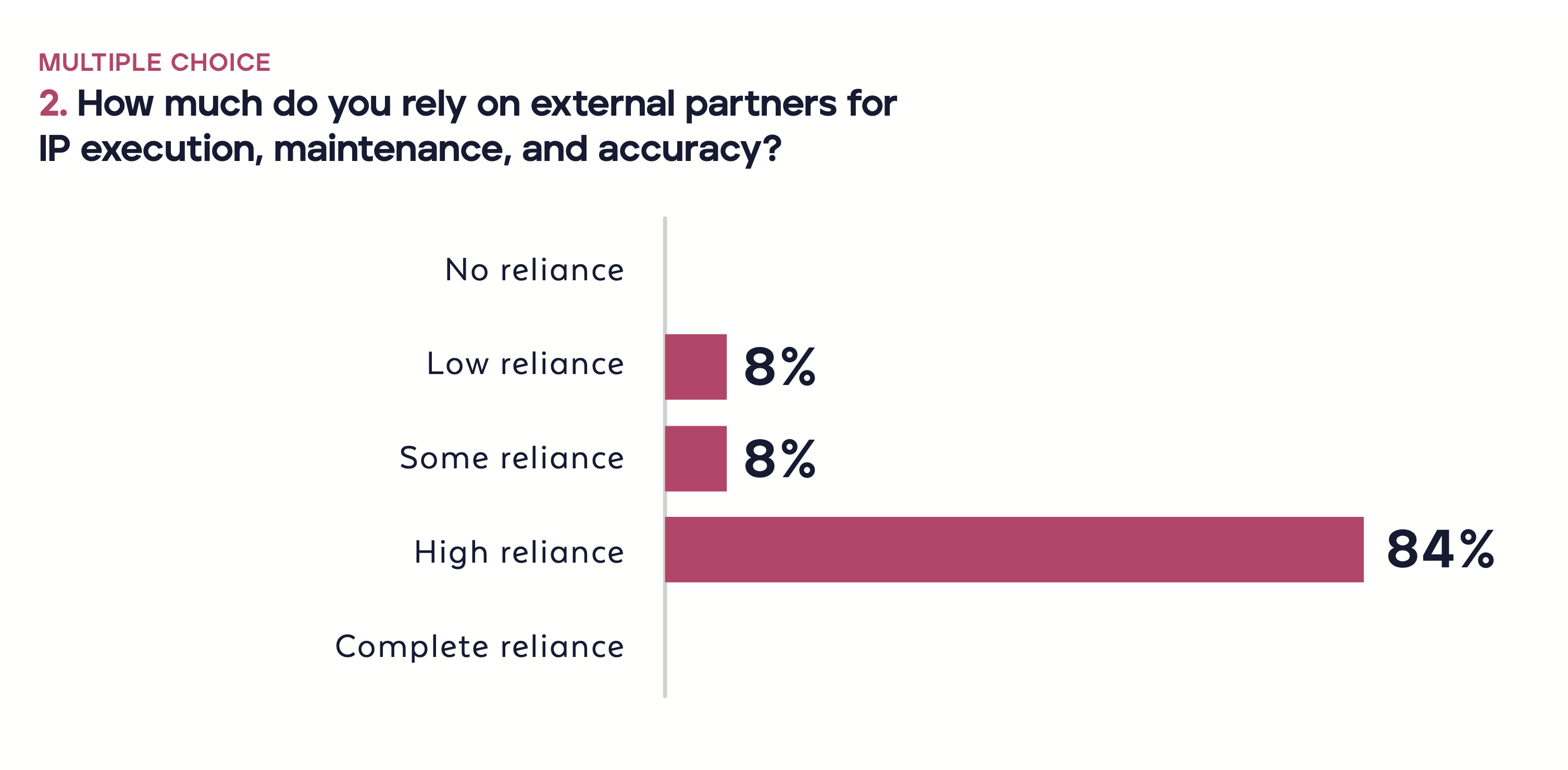
We also found that 84% of the webinar participants heavily depend on external partners for managing intellectual property (IP). Relying on third-party vendors for important tasks like editing and rule creation can lock health plans into external systems and processes—making it more difficult to adapt to meet new regulations or adopt new systems.
Involved third-party partnerships can also become less cooperative, leading to external vendors benefiting from recurring problems instead of working together to solve them. Plus, depending on external vendors can be more expensive and introduce security risks over time.
 The Advanced Custom Edits (ACE) solution from HealthEdge Source™ puts the power back in your hands by offering an advantage over traditional approaches to payment integrity. With ACE, your health plan can create edits that are tailored to specific organizational policies and data. This means you won’t have to wait through lengthy development cycles or use more of your budget for external help. Plus, you have complete control over the final product, ensuring it aligns perfectly with your plan’s unique needs.
The Advanced Custom Edits (ACE) solution from HealthEdge Source™ puts the power back in your hands by offering an advantage over traditional approaches to payment integrity. With ACE, your health plan can create edits that are tailored to specific organizational policies and data. This means you won’t have to wait through lengthy development cycles or use more of your budget for external help. Plus, you have complete control over the final product, ensuring it aligns perfectly with your plan’s unique needs.
No one knows your data and policies better than your team. The ACE solution recognizes this and provides the efficiency and flexibility your plan needs to take ownership of your payment integrity processes. By empowering your team to create their own edits, ACE fosters a more collaborative and solution-oriented approach that leads to greater accuracy, efficiency, and cost savings.
Benefits of Advanced Custom Edits from HealthEdge Source™
HealthEdge Source™ is the ultimate solution for payment integrity. It seamlessly integrates with existing adjudication systems, providing a centralized platform to manage all your health plan’s editing requirements. Whether you require standard, custom, or third-party edits, Source efficiently handles them all with speed, accuracy, and transparency. Additionally, Source offers powerful analytics and reporting features to monitor your payment integrity performance.
Advanced Custom Edits are accessible through the Source user interface, equipped with all the familiar functionalities of Custom Edits. This point-and-click tool allows you to effortlessly create complex edits in the user interface, test the edits, and activate them in just minutes. Whether you need to rectify billing errors, modifier abuse, frequency limits, duplicate claims, downcoding, or any other payment integrity issue, you can accomplish it all with ACE.
The Advanced Custom Edits tool is here to put control back in your health plan’s hands. Some of the primary benefits of leveraging ACE include:
- Build edits based on your specific policies and data without waiting on external vendors or paying hefty fees.
- Create and update edits in minutes, without involving IT resources, to keep pace with changing regulations and policies.
- Ensure your edits are tailored to your health plan’s exact needs, minimizing errors and ensuring compliance.
- Prevent overpayments, underpayments, and fraud, saving you time and money.
- Easily understand how your edits work and share them with your team for better collaboration.
Benefits of Advanced Custom Edits from HealthEdge Source™
While there are many benefits of leveraging Advanced Custom Edits, we gathered three of the most valuable ways the tool impacts payment integrity processes for our health plan customers.
Reduce Duplicate Claims
Duplicate claims occur when the same service is billed more than once, either by the same or different providers. This can happen due to errors, miscommunication, or fraud and cause issues like overpayments, underpayments, or unnecessary costs.
With Advanced Custom Edits, health plans can create a duplicate edit that checks or compares any selected field, such as date of service, provider, CPT codes, modifiers, charges, and more. Users can also deny, adjust, and append claims as well as make a simple or complex duplicate edit.
Create Frequency Limits
Frequency limits restrict the number of units, visits, or services that a member can receive in a certain time period. They are based on medical necessity, clinical guidelines, or contractual agreements and can prevent overutilization, waste, or abuse.
With ACE, you can create a frequency edit to identify claims that exceed your frequency limits based on internal policy and data. Users can filter by fields such as CPT codes, modifiers, revenue codes, and providers, in addition to using different operators, such as equals, less than, greater than, etc.
Identify Downcoding
Downcoding is a practice where a provider bills a lower level of service than what was actually provided, or what was documented in the medical record. It can happen due to errors or misunderstanding. It can result in underpayments, compliance issues, or quality concerns.
With ACE, you can create a downcoding edit that detects claims that have a mismatch between the facility and the physician level of service, based on your policy and data. Like with Frequency Limits, users can filter by CPT codes, modifiers, type of bill, providers, as well as operators like equals, less than, or greater than.
Frequently Asked Questions about Advanced Custom Edits
How do users test the edits that you create with ACE?
Users can test the edits in several ways:
- Monitor Mode: Observe how your edits perform on live claims without affecting the adjudication process.
- Batch Processing: Run claims against your edits in bulk.
- Manual Claim Portal: Enter claims manually to see the results.
- Analytics and Reporting: Track and measure the impact of your edits.
How do users document or share the edits you create with ACE?
Use the notes feature within the tool to document or share edits:
- Add Notes: Include links, references, or any other relevant information.
- View Notes: See notes added by other users, including the date and user name.
- Audit Trail: Create a detailed audit trail and collaborate with team members and stakeholders.
Are there limitations or special permissions needed to access ACE?
There are no specific limitations or special permissions required to access Advanced Custom Edits. It is designed to empower teams to manage their own content and intellectual property.
Can you provide more information on how advanced custom edits can help reduce dependency on external partners?
The ACE tool reduces dependency on external vendors by allowing teams to enact their own policies, create custom edits specific to their needs, and centralize the payment integrity process by eliminating the need for new editing and post-pay vendor solutions.
Is ACE a replacement for existing custom edits or a new separate feature?
Advanced Custom Edits is a new feature developed to provide advanced custom editing capabilities. It enhances existing custom edits by offering more control and customization.
The recent HealthEdge webinar provides valuable insights for health plans seeking to improve payment integrity and reduce dependence on external vendors. The session provided information on payment integrity topics vital to many health plans, such as billing errors, modifier abuse, frequency limits, duplicate claims, and downcoding.
