Value-Based Reimbursement: Collaboration Required to Lower Costs and Improve Care
Our recent consumer survey showed that 47% of the 3,000 respondents postponed care. And of that 47%, 55% delayed routine visits, 39% elective treatment, 32% essential treatment of a chronic condition and 22% emergency care. This might be slightly elevated because of the fear factor related to COVID-19, but many people may not be aware that consumers postpone care all the time. Many times, it’s because of the desire to avoid high costs.
So, it’s no surprise that when asked what services would improve the consumers’ current level of satisfaction with their health plan, tools or information to help understand benefits and financial responsibility (55%) and to help find less costly care (49%) topped the list. Confusion continues beyond just transactions and expenses; the consumer survey also found that 50% of insured American adults don’t know all the services covered under their health plan.
Value-Based Reimbursement Collaboration is Essential for Keeping Members Healthy and Lowering costs
Confusion around health insurance costs and coverage leading to delayed care is critical for payers to address because healthcare is changing, and the focus is shifting to quality. As the industry moves to value-based reimbursements, members avoiding care can actually drive costs up. Many regulations are requiring evidence of quality in the hospitals, health plans and clinics, etc. As a result, providers can be rewarded financially for demonstrating quality and keeping patients healthy. The benefit to payors is, if members are kept healthy, costs for everyone can decrease, and member satisfaction can increase.
For a high-risk Medicare member, a health plan might receive several thousand monthly reimbursements from CMS to care for that member. If the member gets sick, the cost of care chips away at that reimbursement. If the health plan and the provider work together and keep that member healthy, everyone benefits, including from a financial perspective. Preventative care and proactive treatment to keep members healthy benefits everyone in the healthcare ecosystem.
The Communication Gap in Preventive Care
Despite the benefits of Value-Based Reimbursement Collaboration, there is still a communication gap when it comes to supporting and promoting preventive care.
According to the consumer survey, when asked if a health insurance company, primary care physician, or a specialist directed the consumer to a community resource like Meals on Wheels or housing assistance to further support their care, 72% said no, including 83% of Medicare Advantage members and 77% of Medicare members.
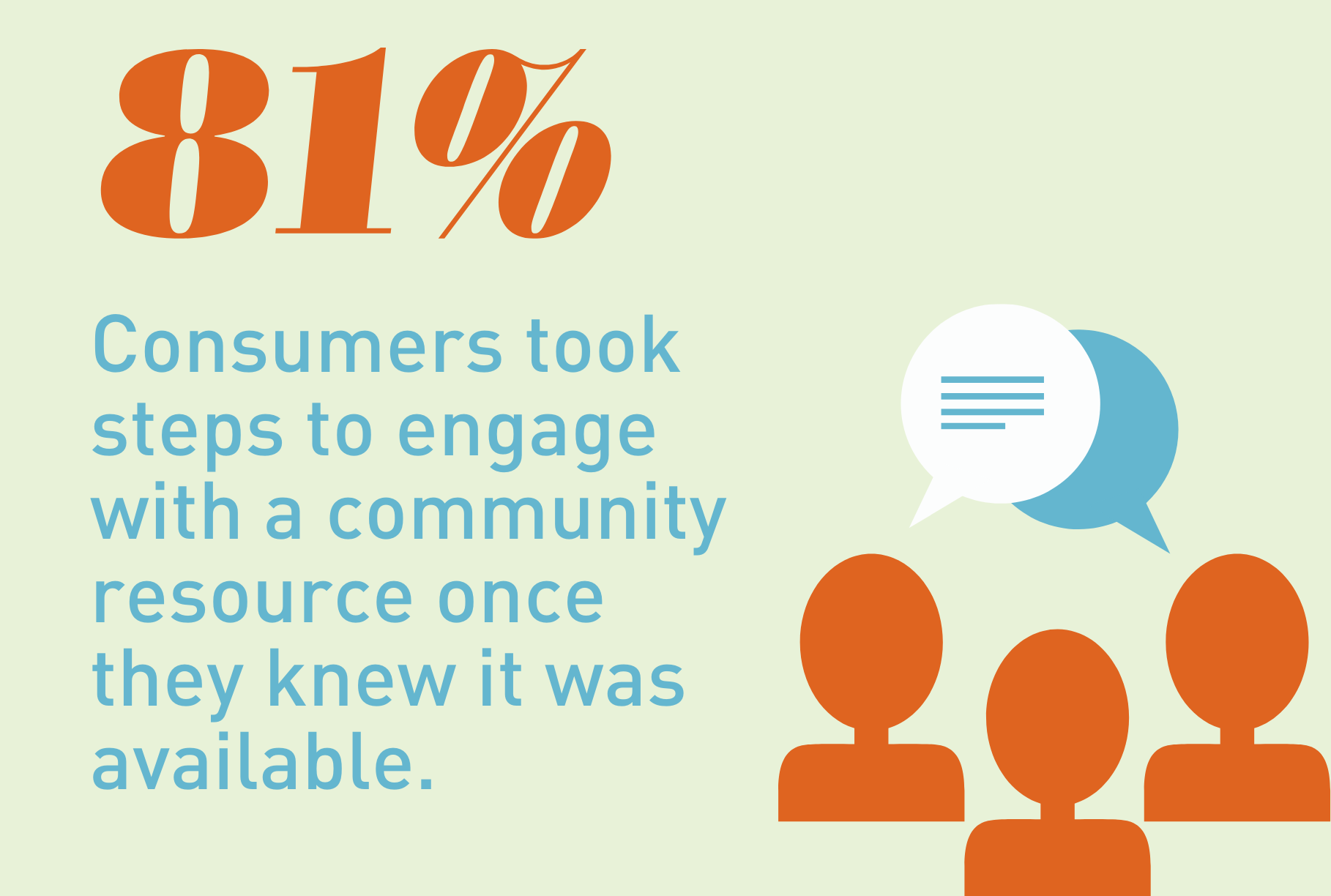
“There is a significant communication gap and missed opportunity for the most vulnerable populations to take advantage of the resources available to help improve their care and overall well-being. There is also evidence that consumers will use these resources if they know they exist. For those directed to community resources, 81% engaged with the services—up from 57% in 2019.”
Consumers want tools to understand their costs, benefits covered, community resources, and overall better communication; if payers and providers work together to improve outreach and overall transparency, it will keep members healthy, lower costs, and benefit everyone in the long run.
