Stop Recurring Post-Payment Issues with an Open Book Approach to Payment Integrity
 At HealthEdge, disrupting the status quo is part of who we are. When it comes to redefining payment integrity, we often think about it in terms of shifting from a black box to an open book approach—essentially empowering payers with technology that enables them to gain control of their IT ecosystems, address root cause issues, and reduce waste in the healthcare system.
At HealthEdge, disrupting the status quo is part of who we are. When it comes to redefining payment integrity, we often think about it in terms of shifting from a black box to an open book approach—essentially empowering payers with technology that enables them to gain control of their IT ecosystems, address root cause issues, and reduce waste in the healthcare system.
But what does that mean? What does reducing waste and abrasion actually look like?
Here’s an example:
Say a patient sustains an injury to their foot and leg and has multiple diagnostic images taken by the same provider on the same day.
The claim they submit to the payer might looks something like this:
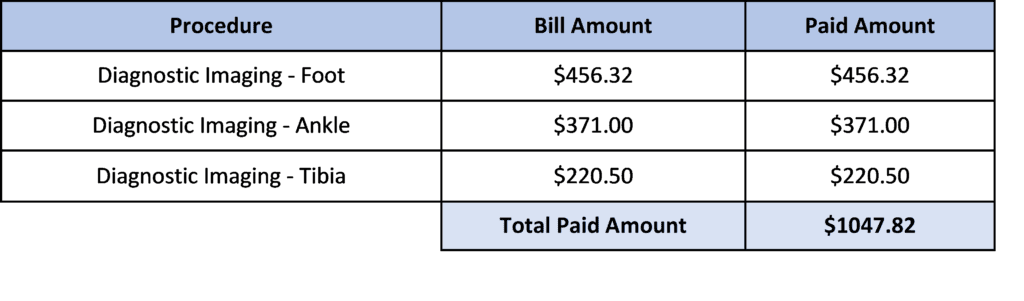
All claim lines are paid at 100%.
After a few months, the claims are reviewed post-payment by a payment integrity vendor. The vendor determines that these procedures are related and should be reimbursed based on multiple procedure payment reduction (MPPR) regulations.
The claim should have paid as follows:
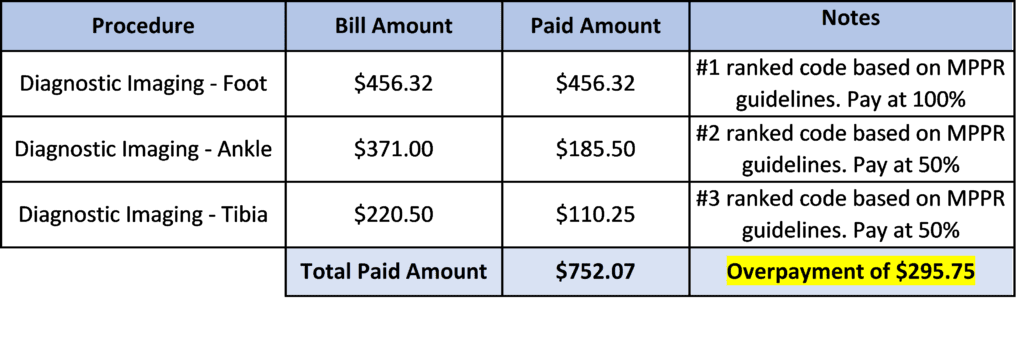
After confirming the overpayment, the following steps are required:
- Payer resources are required to validate the findings for the existing vendor.
- The vendor notifies the provider and attempts to recover the overpayment of $295.75
- Note – Post-payment vendors are only able to recover 60-70% of identified overpayments
- The vendor charges a contingency fee of 15-20% on the recovered savings
- The payer then needs to reprocess the corrected claim.
In this type of payment integrity environment, the above example can occur at a very high volume. Additionally, traditional payment integrity vendors identify this type of issue on a recurring basis but never address the root cause issue—so the overpayments, administrative burden, rework, and provider abrasion continues.
When we talk about striving for accuracy, we’re talking about shifting processes upstream so that claims are paid quickly and comprehensively the first time.
With Source, the above example would be handled differently.
Instead of the claim being passed through pricing and then editing, Source provides integrated claims processing of policy edits, pricing algorithms, and rate schedules. We call this function parallel processing, and it unlocks the ability to view and assess a claim more holistically.
In this scenario, through parallel processing of MPPR edits and reimbursement content, the line level reductions would be applied prior to payment. The root cause of the recurring issues would be addressed at the earliest possible intervention point.
Reimbursing accurately and upstream provides the following benefits:
- Elimination of overpayments
- Avoidance of contingency fees to the existing post payment vendor
- Resource savings for all payer employees involved in the rework of claims
- Reduction of provider abrasion
With Source, you not only have complete control and visibility over your payment lifecycle in one place, but a dedicated partner who wants to help solve your largest and most complex payment challenges. We want to eliminate administrative waste and provider abrasion so that payers can focus on what matters most—their members.
“…if we redefined payment integrity as not recovery, but intelligence striving for accuracy, people’s thought processes would change. If people change the way they think about payment integrity, it will start to inspire people to work on improving the system….” – Ryan Mooney, GM & EVP of Payment Integrity at HealthEdge
