3 Critical Care Management Market Drivers
At HealthEdge, we keep a close eye on the market and the drivers that are influencing healthcare. Our team looks to the experts at Gartner and KLAS, surveys our clients to understand what they’re doing, engages with client’s clinical staff to understand how they use our tool set, and monitors the marketplace to meet the needs of our customers.
These are the top 3 care management trends we’re seeing:
- Doing more with less
Remaining competitive in today’s market means optimizing healthcare operations so clinicians can remain focused on caring for member populations.
One of the trends in the healthcare industry is the decrease in people entering the profession, especially nurses, which is going to lead to a significant shortage. This is further compounded by the Great Resignation and high turnover rates which add to the shortage. At the same time, we’re seeing an increase in the number of people who are developing a chronic illness, which is driving the need for us to make our tools much more efficient so we can care for members. With less staff – especially in a value-based environment – we need tools to help health plans do more with less.
One of the things we’re excited about at HealthEdge is our digital care member outreach platform. This helps your clinical staff be far more efficient by putting some of the work that the care manager does in the hands of the member to enable their own engaged, active participation in managing parts of the care management continuum.

Source: 20% nurse shortage, 171 million people with one chronic condition
- Increasing Demand for Interoperability
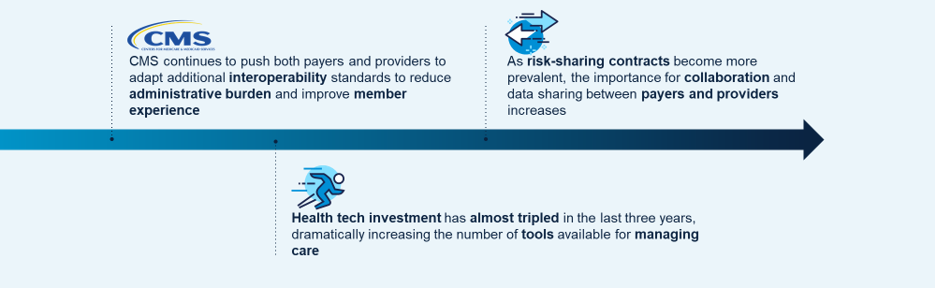
Another trend we’re seeing is an increased demand for interoperability among solutions. Regulatory pressures, the shift to digital health, and new payer-provider business models underscore this growing need.
The main drivers include:
- Government agencies such as CMS are continuing to push payers and providers to increase the interoperability between their systems. This is to reduce administrative burden and errors, as well as improve the overall member experience.
- We’re also seeing a lot more collaboration demand between payers and providers. This is driving a lot of data exchange requirements, such as integrating our solutions with electronic health records, and building real-time interfaces with our clients’ data infrastructure so that we can exchange data between these systems in real time.
- The underpinning of all of this is an explosion of health technology.
- The Importance of a Modern Platform
Payers are embracing next-level platforms with connected ecosystems and real-time data insights that impact cost and quality outcomes. According to a recent McKinsey article, Cloud capabilities have the potential to generate value of $100b to $170b in 2030 for healthcare companies.
There are five healthcare categories that benefit from cloud technology:
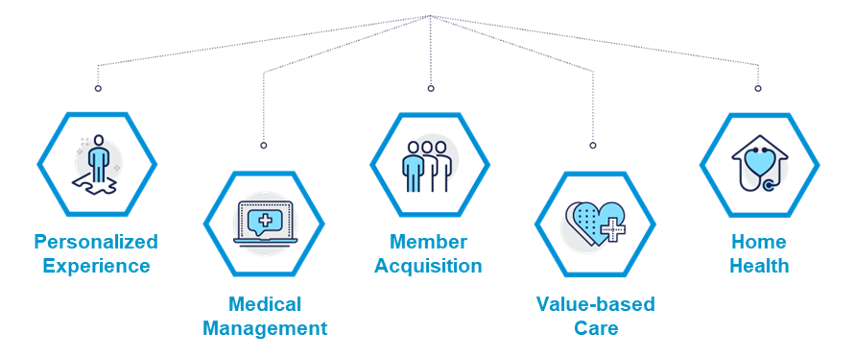
By 2024, healthcare providers that have adopted a Digital Health Platform will outpace competition by 80% in the speed of digital transformation and new feature implementation.
HealthEdge: The Right Platform
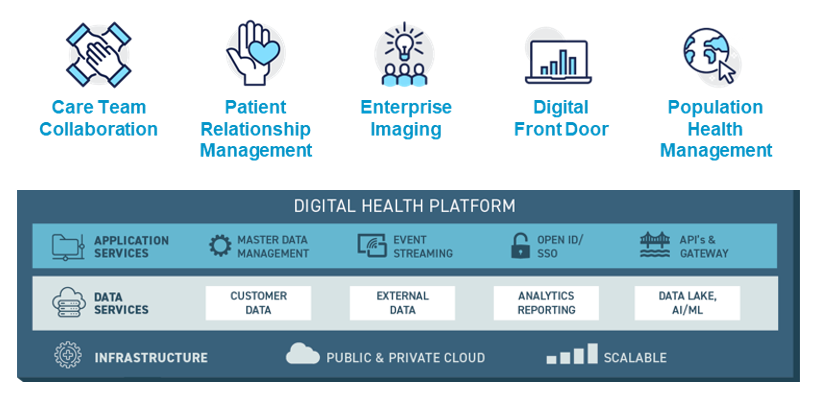
To remain viable in the evolving industry, health plans must lean into the above drivers and opportunities, rather than ignoring them. Thus, you need the right platform underlying your systems, and you need to take some steps to build a strong foundation that aligns with where the market is heading.
This is the thesis of HealthEdge and the GuidingCare team – to build a digital health plan ecosystem with best of breed products: core admin (HealthRules Payer®), care management (GuidingCare®), prospective payment integrity (Source), and member experience (Wellframe).
