6 Distinct Advantages of Real-Time for Health Plans
Background
Many health plan customers have historical workflows that rely on batch processes – file a claim on Day 1 and the results are available on Day 2 (or 3 or 4). Because of limitations with compute, storage, and network performance years ago, the idea of processing a piece of information in milliseconds was unheard of, primarily since it was not technically feasible to do it in a cost-efficient manner. However, in 2022, real-time, scalable, and global systems are commonplace.
Innovative companies across industries have taken advantage of these disruptive trends to deliver seamless, digital experiences that we take for granted today -– when we buy with 1-Click on Amazon or watch our Uber driver inch his or her way along the map on the way to pick us up. These become the baseline expectation. If you are the consumer of health insurance, you also expect to participate in these experiences. If you are the provider of that health insurance, you are expected to deliver this experience.
Real Time APIs (for Business Outcomes)
HealthRules Payer (and all HealthEdge products) are designed with real-time APIs. It is one of the reasons why Payor continues to be a Gartner Next-Gen solution for the Core Admin Processing Systems market. This is now table stakes for participating in this market and the baseline of our customers, who are modernizing for the coming decade.
Real-time APIs are the product that close the gap between various cloud-based health systems (CAPS, EHR, Pop Health, Portals, Mobile) and enable new experiences for members, providers, and users of these systems. Today, customers leverage the rich suite of real-time APIs to power member portals, send out correspondence, or determine member costs before they go to the hospital for a procedure. For example, HealthRules Payer real-time Trial Claim API allows for health plans to meet the government mandate for member specific pricing and cost sharing through the price comparison tools, as well as the AEOBs (Advanced Explanation of Benefits)
Real Time Events (for Business Outcomes)
The next stage of evolution for HealthRules Payer’s (HRP) integration capabilities is real-time event streaming, which is sometimes called stream processing. It sounds technical – but is conceptually easy to understand – and it solves some of the challenges that current businesses require to be even more responsive to customers. Created by LinkedIn over a decade ago and managed, now, as open source by Apache, Kafka is a technology used by most Fortune 100 companies to help with business events that occur thousands, millions, or billions of times per day (e.g., data from IoT (Internet of Things) device, a new member enrollment, LinkedIn message posts).
To achieve this, Kafka uses what is called a publish-subscribe messaging architecture. At the core of Kafka (and event streaming in general) is the concept of an “event” – i.e., something happened. It could be that a member got enrolled, a claim has been paid, or a heartbeat on a heart rate monitor exceeded a threshold. These events in small quantities or millions are “published” by applications (also called “producers”) and are “subscribed” to by downstream applications that need this information (also called “consumers”). And these events can be organized into logical “topics”. So, events related to enrollment go in one stream and events related to billing, perhaps, another. If each published event were a 3×5 card with information, those events are placed on to one of many user-defined conveyor belts in time order with each conveyor belt reflecting that different topic.
As a concrete example, an event could be a new member has enrolled for health coverage. As the source application, HRP “publishes” this event to the “Membership” topic. Any downstream application such as a correspondence solution for member ID cards or a member portal can “subscribe” to this topic. A depiction of this architecture is given below. If you want the fun, non-technical, children’s storybook illustration of how this works, please check this link out. It’s very well done.
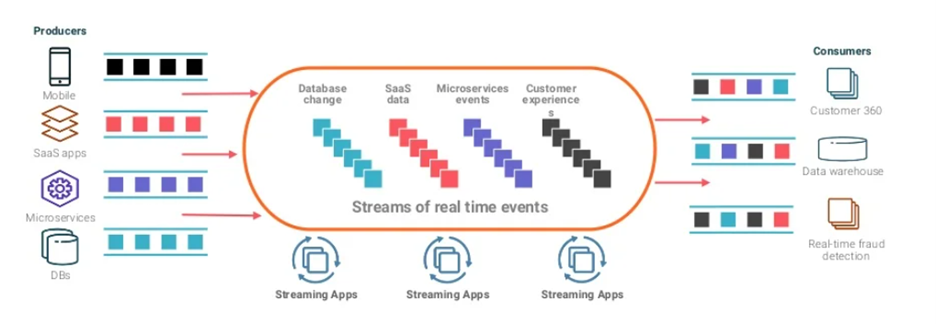
HealthEdge’s objective with creating a Kafka-based event streaming architecture is to help our customers achieve digital transformation by democratizing the data in the HealthRules ecosystem, allowing them to leverage the power of “real-time” healthcare data to build modern, digital, world class experiences for their members.
Unique Capabilities and Use Cases
Because health plans are an ecosystem of integrated solutions with a CAPS at the core, there are some distinct advantages of this real-time messaging system that are especially relevant for payers:
Fault Tolerance – Because event producers and consumers are effectively de-coupled through this event streaming service, HRP can continue to publish events even if consumers are not online and vice versa. The events are backed up and consumed when the consumers come back online.
Performance – Kafka is extremely low latency (fast) and scales (powerful) to support millions or billions of events without impacting the core performance of HRP. Customers can continue to add events and topics with any number of consumers downstream and not impact HRP’s performance.
Highly Configurable – Instead of each additional use case for real-time data from HRP (and other HealthEdge products) needing an integration project or custom APIs, customers can use (and re-use) the same topics and published events across various consumers and configure these streams through a web UI.
Healthcare payors can configure and consume different data streams for a wide variety of use cases … use cases that we’re familiar and newer ones afforded by the performance and reliability:
Connecting with enterprise apps or other internal systems – Payors can use these data streams to connect to customer/provider service apps (enabling real-time response to customer and provider issues) or CRM (Customer Relationship Management) systems like Salesforce or to power new-age apps like chatbots.
Power their own AI/ML algorithms – The scale and reliability of these data streams enable payors to use them to power their custom ML models for complex use cases like fraud detection.
Analytics or dashboards – Customers with their own centralized analytics and dashboard capabilities can use the data streaming through topics to power these dashboards in real-time with claims, member and other HRP data.
A Step Ahead
Real-time experiences for members and providers are both here today, but also growing in sophistication and complexity to push the art-of-the-possible. HealthEdge is committed to keeping our customers a step ahead in delivering these experiences through evolving technologies applied to business outcomes.
Learn more about HealthRules Payer here.
