Converge Without Limits
What does it mean to converge without limits?
While the science of care has advanced tremendously, health plans are still waiting for the breakthrough innovations that will transform the way they use data to communicate with members, collaborate with providers, improve care and make smarter business decisions.
HealthEdge is out to change that.
We have the integrated platform – and the vision – that will enable health plans to combine all their clinical and administrative data so they can break down the boundaries that are holding them back.
With that level of access, your plan can:
– Leverage automation to enhance care delivery, efficiency and compliance
– Increase the speed and accuracy of payments
– Deliver a level of service your members have come to expect
– Gain the next-level insights that will pave the way to smarter, healthier and less costly member care

Transforming payer relationships at all levels
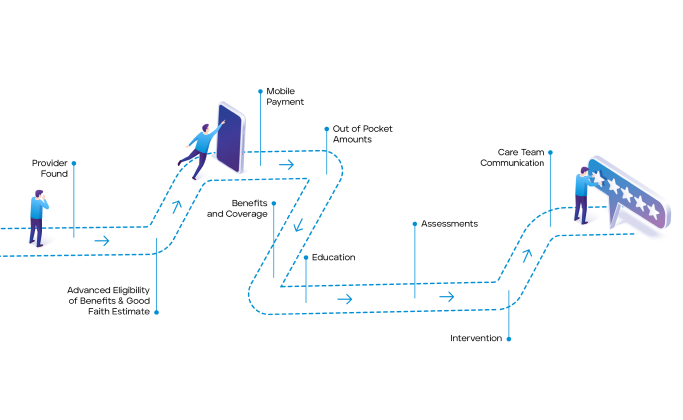
The Member Experience
Instead of disjointed, confusing interactions via traditional means (telephone, emails, portals), members can choose to access powerful self-service tools or engage directly with highly informed representatives via the same modern means they’ve come to expect from their retail experiences with companies like Amazon and Google.
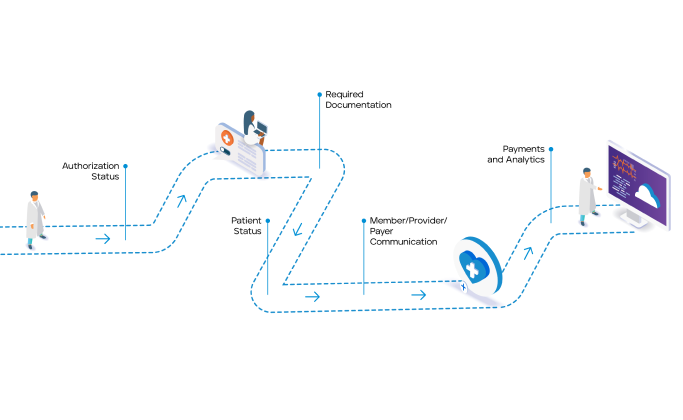
The Provider Experience
Instead of manual-intensive interactions with payers that are stifled by latent data and lengthy authorization and claims payment processes, providers can get instant access to real-time data on patient benefit plans to expedite care and optimize health and financial outcomes for everyone.
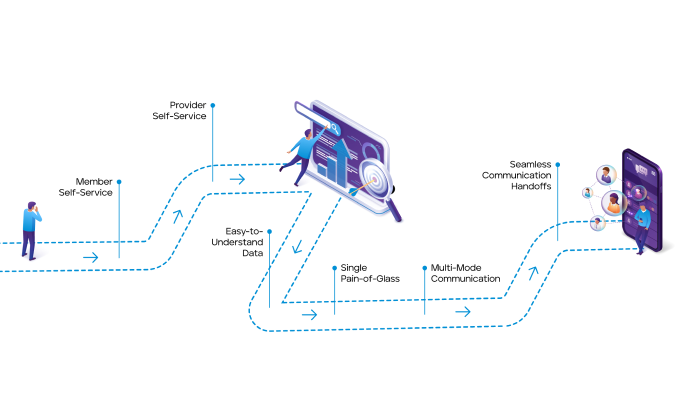
The Member Services Experience
Instead of wasting hours on hold and struggling to get complete answers to provider and member questions, member service reps can offload repetitive workloads to automated digital healthcare software and spend quality time triaging the exceptions – all from a single screen that presents the right information at the right time.
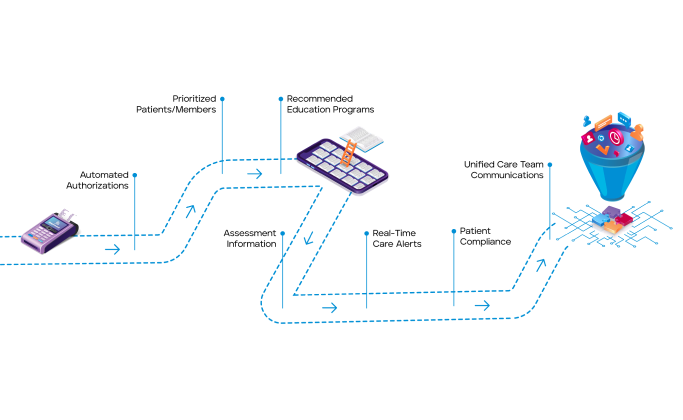
The Care Manager Experience
Instead of hunting for member data across multiple systems to support member needs and compliance requirements, care managers can easily get a real-time picture of member activity from IoT devices and clinical SMEs to optimize care plans and engage members more holistically.
A new era for health plans
By using our digital healthcare software to automate business workflows and seamlessly exchange data in real time across the ecosystem, HealthEdge customers experience the business attributes of improved end-user and consumer centricity, ever-reducing transaction costs, ever-increasing quality and ever-increasing service levels and business transparency.
Case Study: How HealthEdge®’s HealthRules® Payer helped Medica transform claims operations through strategic automation
When Medica wanted to leverage the benefits of automation for claims processing, they partnered with HealthEdge. We helped them significantly accelerate processing while dramatically reducing costs.
READ CASE STUDY



