From rapidly changing regulatory requirements and new competitive forces to changing payment models and rising consumer expectations, 2024 is shaping up to be another challenging year for health plans. In this 5-part blog series entitled HealthEdge Horizons, we dive deeper into the trends that are shaping our industry and explore how HealthEdge solutions are helping payers address their biggest challenges head-on. Be sure to check out the entire series:
The Origins of Value-Based Care
Since the Institute for Healthcare Improvement (IHI) first articulated the Triple Aim in 2008, the healthcare industry has undergone a massive transformation over the past 15+ years, shifting from paying for services (fee-for-service or FFS) toward paying for quality (value-based care or VBC).
Initially, the Triple Aim provided a framework for “optimizing health for individuals and populations by simultaneously improving the patient experience of care (including quality and satisfaction), improving the health of the population, and reducing per capita cost of care for the benefit of communities,” according to the IHI. Several years later, it evolved to include a focus on the well-being of the healthcare workforce and advancing health equity, with some now referring to it as the Quintuple Aim.
With the passing of the Affordable Care Act of 2011, the concepts of healthcare providers and payers working together to embrace quality finally began to take hold. However, when the existing FFS payment structure was put to the test in the Medicare Acute Care Episode (ACE) Demonstration Project in 2018, the feasibility of value-based care became apparent. It ushered in a new era of bundled payment initiatives, including what we now know as value-based care.
The Financial and Care Incentives
Value-based care introduces financial incentives for healthcare providers to ensure patients stay healthy. Under this model, providers are financially rewarded for maintaining their patients’ well-being. The key lies in value-based contract arrangements that distribute funds to providers at a broader level, such as a “bucket” or global level.
When patients remain healthy, cost savings are shared with the provider, creating a win-win situation. Patients benefit from improved health, lower expenses, and better care coordination. Providers are incentivized to focus on preventive care and wellness, as it directly impacts their financial compensation. In this way, value-based care aligns the interests of patients, providers, and payers.
Value-Based Care Today
So, where do VBC payment models stand after all of these years? According to a May 2023 Healthcare Payer Intelligence report, CMS recently reported successfully linking 90% of payments to value, and 40% of all payments flow through alternative payment models (APMs). While the rest of the healthcare industry is transitioning toward value-based care contracts, fee-for-service arrangements still represent a significant portion of the market. However, administering these contracts and transitioning from traditional models to value-based care has proven challenging. This is where modern technology, like HealthEdge solutions, comes into play.
The Role of Modern Technology
Transitioning from fee-for-service to value-based care requires a fundamental shift in managing and reimbursing healthcare. Traditional systems designed for fee-for-service models must adapt, but unfortunately, many legacy and outdated systems cannot support this transformation.
It’s one thing to say you are going to move from fee-for-service to value-based care, but it is another to administer the many different forms of value-based care, such as shared-risks, capitated arrangements, and many different forms of bundled payments.
How do payers take a traditional system that was designed for the model of “patient gets sick, patient goes to the doctor or hospital, a hospital gets paid, repeat the cycle” and convert it to supporting new models that tie reimbursements to patient outcomes and experiences with the doctor/hospital?
The answer: They can’t. Modern, flexible systems are a must-have in value-based care.
A Brighter Future with Value for All Stakeholders
HealthEdge recognizes the need for an integrated approach that combines contracting, claims administration, and care coordination in a single entity. This holistic approach ensures that the financial and care components of value-based care align seamlessly. With HealthEdge’s ecosystem of these three essential components, payers can efficiently manage value-based care programs and control costs effectively.
With HealthEdge, digital health plans have a unique opportunity to make this transition highly successful for all stakeholders: payers, providers, and patients. They can do so by leveraging the advanced automation capabilities and real-time data insights readily available in modern core administrative processing systems (CAPS) like HealthRules® Payer. With the right CAPS in place, the value of value-based contracts becomes crystal clear:
- Cost Control: Value-based care models can help health plans control costs over the long term by focusing on preventive care and early intervention
- Improved Member Health: By promoting healthier lifestyles and proactive healthcare management, value-based care can lead to improved health outcomes among members. This enhances members satisfaction and reduces the financial burden on payers.
- Competitive Advantage: Payers that embrace value-based care early gain a competitive edge. They can attract providers and members who appreciate the benefits of this approach.
Here are a few practical examples of how all HealthEdge solutions are helping health plans navigate this transformation successfully, improving patient outcomes and reducing healthcare costs in the process:
- HealthRules® Payer
- Agile & flexible HealthRules Language
- Quickly configure new benefit plans and contract arrangements
- Share actionable data
with stakeholders
- Make value-based reimbursement & improved customer satisfaction a reality
- Up to 96% billing accuracy, including with complex value-based agreements
- Learn more about our core administrative processing system.
- HealthEdge Source™ payment integrity platform
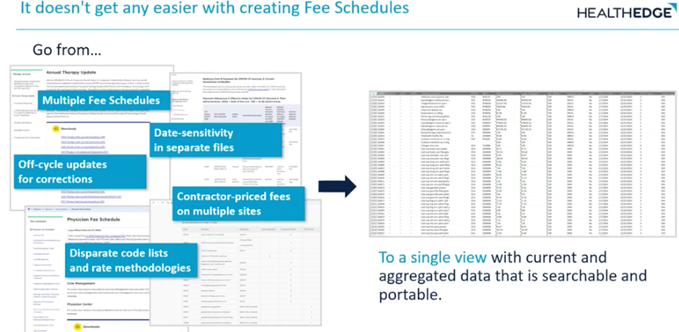
- Accurately price claims based on complex contractual arrangements
- Run in parallel with fee-for-service contract terms
- Handle both prospective and retrospective bundles
- Enable predictive modeling and impact reconciliation reports
- Learn more about our payment integrity platform.
- GuidingCare® care management platform
- Facilitates complex workflows to manage care plans in value-based arrangements
- Intuitive gaps-in-care analytics identify high-risk patients and potential health improvement opportunities
- Evaluate performance across configurable measure sets such as HEDIS and Star ratings, plus state and custom measure sets
- Learn more about our care management platform.
- Wellframe member experience platform
- Assigned programs focus on whole-person health and improved care outcomes
- Proven ROI in utilization management outcomes, with a 17% reduction in inpatient admissions** and a 23% increase in preventive medicine utilization**
- Builds framework for assessing target population and managing clinical needs
- Learn more about our member experience platform.
Health plans that want to remain competitive and win new business need to support value-based arrangements at every touchpoint in their ecosystem and have access to relevant data outputs for internal and external tracking and analysis.
To learn more about how HealthEdge solutions can help your organization successfully implement value-based care, visit www.healthedge.com.