The one with the best data typically wins, right? We’ve seen it happen time and time again in our personal lives and in other industries.
If you are a parent of a teenager, you know that the data you’ve collected over the years of being an adult typically makes you a more informed decision maker than your teenager.
And just think about the amount of personal data Facebook has on its users or the amount of professional data LinkedIn can access about its users. The more data these social media platforms have about you, the more successful their advertisers will be, which ultimately results in more ad dollars being spent on the most effective platforms. The greater the data, the greater the success.
This same concept holds true in the healthcare industry. Those who are able to embrace the massive amount of healthcare data being generated by the digitization of healthcare are the ones who are most likely to succeed. Health plans that can use their data to automate more businesses processes, build better experiences for providers and members, and make smarter business decisions are the ones with the competitive advantage.
Data is Everywhere
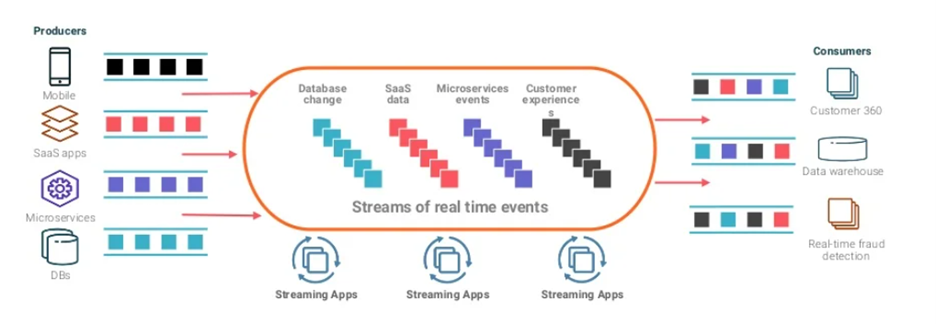
All different types of healthcare data are funneled into payers from everywhere and at all different intervals. This includes everything from a member’s Apple watch to remote patient monitoring devices, claims administration systems, and even unstructured provider clinical notes. But how can health plans leverage this data to create competitive advantages and thrive in the new age of digital healthcare?
The secret is in the IT systems they choose. Building a solid foundation of workflows and business processes based on accurate, timely, and complete data that is centralized and managed efficiently is at the core of successful health plans. Let’s take a look at what good data can do.
For example, with a modern claims payment processing system like Source, health plans can:
- Adjudicate more claims correctly on the first try: By leveraging claims edit data to identify and resolve issues earlier in the adjudication process, fewer claims require rework and more claims get processed correctly on the first pass. This translates into lower transaction costs and higher margins.
- Automate more of the claims payment processes with new workflows, such as prior authorizations, because they trust that the data is accurate and is going to drive smarter processes that require fewer manual touches. This translates to lower risk of human error and helps reduce the burdens brought on by workforce shortages.
- Enable a better provider and member experience. When fewer over-/under-payments are made due to more accurate data, providers begin to trust these payers and can work more collaboratively to facilitate a better member experience. This translates to stronger provider relationships and higher member loyalty.
- Make better business decisions. With accurate and complete data, health plan administrators are in a better position to make more informed decisions. Modern systems, like Source, offer analytics and modeling capabilities that make what-if scenarios possible. Whether it is contract negotiations or adapting to new value-based care payment models, good data makes the difference between well-informed decisions vs. shots in the dark. This translates into better decisions that facilitate smart growth.
Accurate, timely, and comprehensive data can not only help you lower operating costs, but it can also give you insights that can be used to create distance between you and your competitors. And in today’s highly dynamic, rapidly evolving health insurance market, that distance is a welcome sight for many health plans.
Better data
To learn more about how to use your data to create a competitive advantage, check out our latest white paper and see 314 Billion Reasons Why Better Data Wins.