A modern care management business intelligence (BI) platform can play a crucial role for health plans. Business intelligence tools help support quality initiatives, manage population health, and optimize resource allocation for healthcare payers. Payers can utilize integrated reporting capabilities to mitigate risk as well as improve clinical and financial outcomes. In addition, the right business intelligence platform can enable health plans to effectively analyze vast quantities of data and deliver high-quality value-based care.
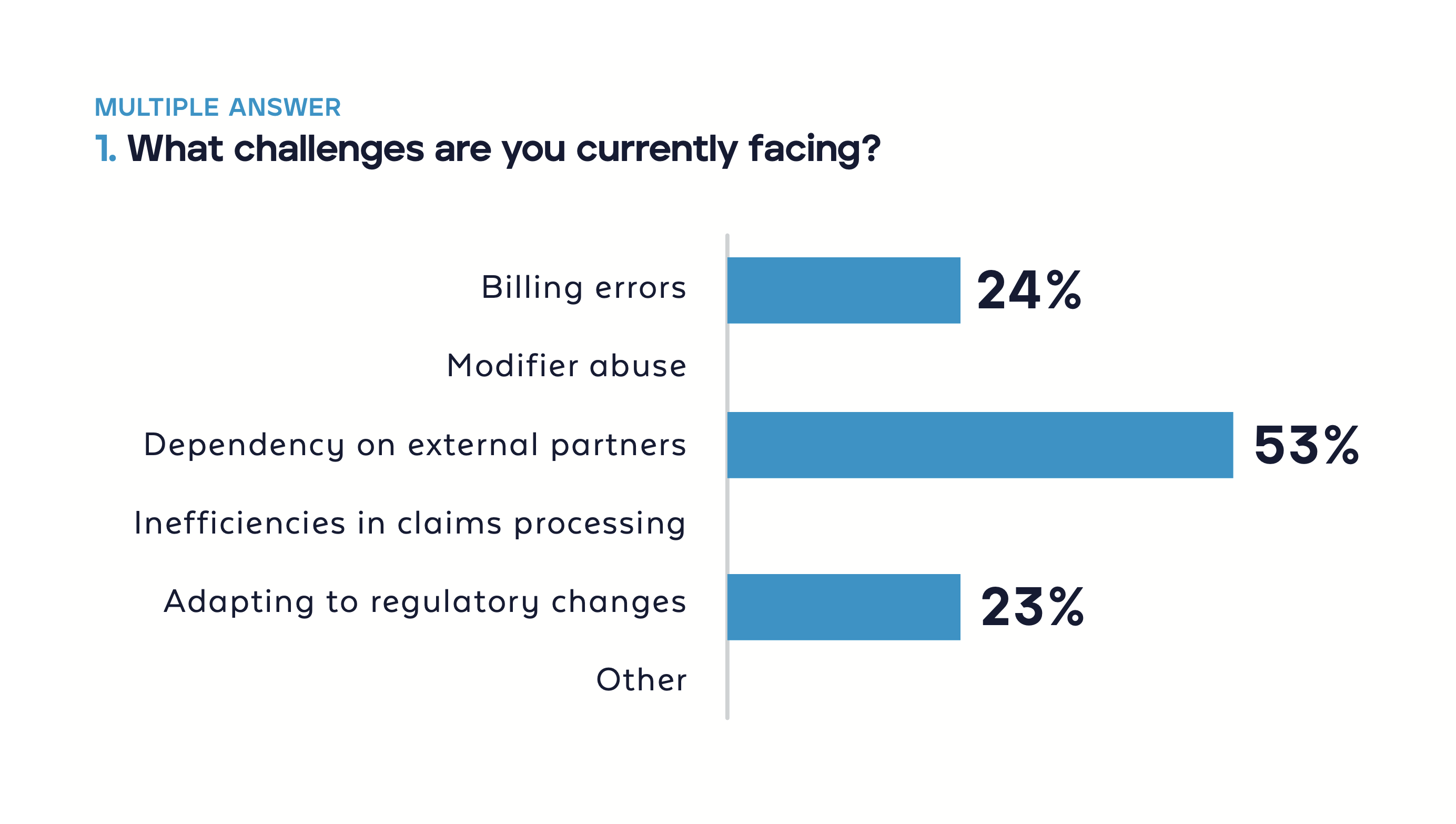
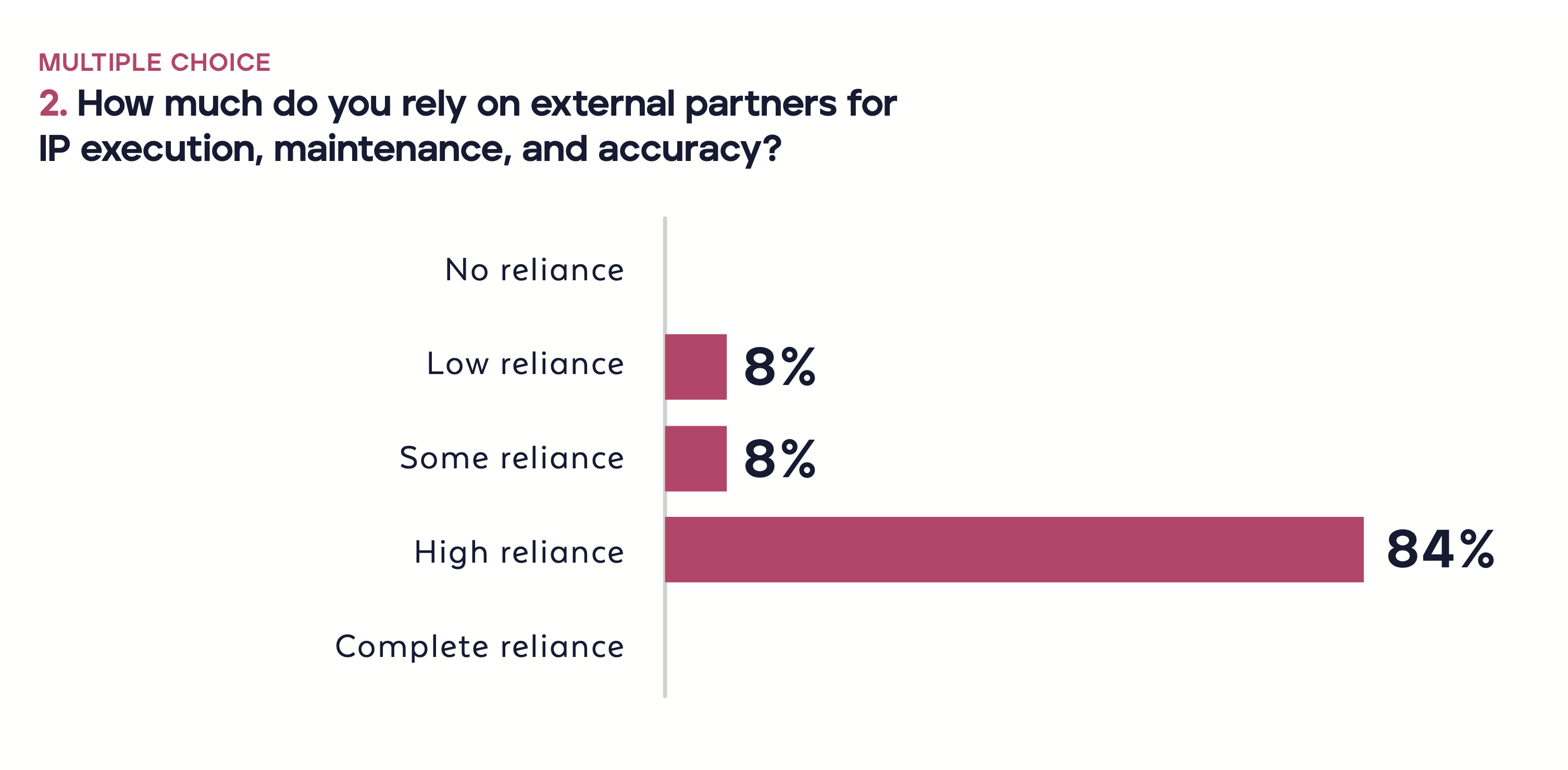
Though there are many benefits to adopting a care management business intelligence platform, health plans may face several common challenges. Many care management solutions lack depth in reporting and analytics, leading to expensive ad hoc solutions. They also tend to fail to integrate clinical and claims data. By using outdated or legacy solutions, health plans often struggle with data overload and limited analytical capabilities, making it challenging to derive meaningful insights from business intelligence.
Today, a new standard in the business intelligence space is necessary to improve healthcare outcomes and operational efficiency.
Key Capabilities for Care Management Business Intelligence Platforms
These challenges can be overcome with health plans requiring business intelligence solutions that are technologically advanced and user-centric. When evaluating care management solutions, health plan leaders should look for platforms that include business intelligence capabilities, which can help:
- Maximize efficiency and minimize costs with powerful, out-of-the-box, and user-friendly reports ready from the moment the solution goes live.
- Provide regulatory support and expertise, including support for regulatory and custom reports to help health plans meet state and federal requirements.
- Leverage data and insights from multiple modules in an end-to-end digital payer solution so that business intelligence can develop a full-picture view of the member, not just the data in the care management system.
Next-Generation Care Management Business intelligence: HealthEdge® GuidingCare®
The Business intelligence Module within the GuidingCare® care management platform from HealthEdge® is a state-of-the-art solution that empowers health plans to elevate their performance. The GuidingCare Business intelligence Module provides a comprehensive view of key information, transforming data into actionable intelligence that payers can use to optimize care delivery and operational efficiency.
GuidingCare Business Intelligence Module
The core Business intelligence Module is a component of the GuidingCare Bundle, supporting health plans to measure outcomes, manage operations, and maintain compliance with ease. The comprehensive reporting and dashboarding solution transforms health plan operations through clinical and operational insights, including capabilities such as:
Standard Reports
- 12 interactive reports covering utilization management, care management, and appeals and grievances use cases.
- Includes operational, trending, and turnaround time data views
- Data and reports can be downloaded in PDF, Excel, and PPT formats
Regulatory Reports
- 20+ Centers for Medicare and Medicaid Services (CMS) regulatory reports covering Organization Determinations, Appeals, and Grievances (ODAG), Coverage Determinations, Appeals, and Grievances (CDAG), and Part C/D needs
- Updated with the latest CMS requirements to support audit and annual reporting needs
- Automatically published to customer environments
Self-Service Reports
- Pre-defined data sources available for self-service report creation
- Robust front-end, database, and data source documentation
- User training provided as part of the Implementation
Advanced Business Intelligence Offerings for the GuidingCare Solution
There are additional premium offerings available so health plans can establish a system according to their unique business needs:
Accreditation Report Suite
Accreditation reporting incorporates HealthEdge’s NCQA expertise, the health plan’s workflow and configuration considerations, and frequently added new reports and enhancements.
- A suite of pre-built reports to support health plan accreditation.
- Includes National Committee for Quality Assurance (NCQA) and Utilization Review Accreditation Commission (URAC) accreditation reports.
- NCQA package that includes 15 reports, updates required per NCQA, minor custom changes, and thorough documentation of business requirements
Premium Report Suite
This reporting suite offers trending reports to help payers make informed business decisions, advanced reports to help tailor services to meet member needs, and additional reports that are frequently updated based on market changes and GuidingCare platform enhancements. A suit of 80+ pre-built and interactive operational dashboards support areas like:
- Care management
- Utilization management and appeals & grievances
- Population health management
- Systems reports
Additional Business intelligence Report Offerings
- Custom Reports and Data Sets: Based on the health plan’s unique reporting requirements, the business intelligence team builds custom reports using their expertise in data modeling and Tableau visualizations.
- Product Training: Our experts provide additional training for health plans on best practices for the self-service tool and in-depth review of the standard report analysis in your environment.
- Additional User Licenses: Purchase additional Publisher and Viewer licenses to expand access to data and insights.
How GuidingCare Business Intelligence Is Different
The GuidingCare Business Intelligence Module stands out with its unmatched standard features and integration of data into actionable reports and analyses. Alternative solutions fail to integrate clinical and claims data seamlessly, and competitor’s standard reports typically lack depth, resulting in a need for ad hoc solutions to bridge these gaps. GuidingCare addresses the complexities of modern health plans’ business by providing a comprehensive solution.
Comprehensive Reporting
GuidingCare offers comprehensive standard reports that help health plans operate more efficiently and reduce business intelligence costs. These reports include quality improvement, preventive, operational, productivity, and trending reports, which provide transparency across the organization. GuidingCare also delivers clinical insights that show changes in risk scores, intervention success rates, and readmission rates by diagnosis-related group, care plan triggers, targeting populations, and program outcomes. By providing insights into gaps in care and the best interventions, GuidingCare helps improve member care and experience.
Seamless Cross-Module Integration and 360 View of Members
GuidingCare has a unique capability that enables seamless integration across various modules such as claims, utilization management, appeals and grievances, care management, and risk management. Unlike other solutions that only report on a specific module, GuidingCare combines all available data into a single comprehensive dashboard. This integration provides a complete view of the authorization process and patient journey, which assists payers in making more informed decisions and improving patient outcomes.
Team of Business intelligence Experts for Support and Customization
The GuidingCare Business intelligence team is a dedicated, certified team that offers premium services in managing, visualizing, and reporting data. The team comprises certified Tableau experts who provide expert technical and domain knowledge to support health plans. They specialize in rapidly creating and testing custom reports with advanced visualizations and ensure that these reports work seamlessly—including when significant system upgrades occur. The Business Intelligence team takes a proactive approach to product improvement and collaborates closely with clinical subject matter experts to ensure data is seamlessly captured and incorporated into workflows.
Operational Efficiency and Compliance
GuidingCare is designed to bridge gaps in care management through prebuilt reports that help health plans improve from day one. Over 20 CMS regulatory reports ensure compliance and aid successful audits. The solution’s self-service capabilities allow quick turnaround times and flexible reporting, further improving operational efficiency.
For more information from a third party on HealthEdge and care management, please see the 2023 Gartner Market Guide for U.S. Healthcare Payer Care Management Workflow Applications.
The Benefits of Next-Generation Business intelligence
Business intelligence in care management is a transformative force that drives strategic decision-making to optimize care and efficiency. Here’s how a GuidingCare Business Intelligence delivers a return on investment for health plans:
Business Impact
- Better insight through analysis of quality initiatives, health management, and allocation of resources.
- Improved decision-making by converting complex data into visualizations showing essential trends and patterns.
- Enhanced care management through population health analytics.
Operational Impact
- Reduce internal business intelligence costs and resource strain with ready-to-use reports at go-live.
- Increase transparency into business insights.
- Improve decision-making and operational efficiencies by helping to identify future and immediate needs.
Regulatory Impact
- Reduce internal resource effort to adapt to regulatory change and support audits with our pre-built CMS regulatory reports available at go-live.
- Reporting is available for review and validation throughout the year.
- Reduced resource needs by having updated reports based on requirement changes.
Modernize Your Business with GuidingCare Business Intelligence
As the healthcare industry becomes increasingly complex, incorporating an advanced care management business intelligence platform is no longer just an advantage but a necessity. GuidingCare Business Intelligence can unlock a new era of efficiency, compliance, and member-focused care. With the right business intelligence capabilities, health plans are better positioned to lead the charge toward a more sustainable, outcome-focused future, ensuring that every decision is data-driven and every care strategy is optimized for success.
To learn more about how GuidingCare Business Intelligence can accelerate your care management transformation, visit our VillageCare case study: Leveraging Business Intelligence to Accelerate Digital Transformation.




 The
The